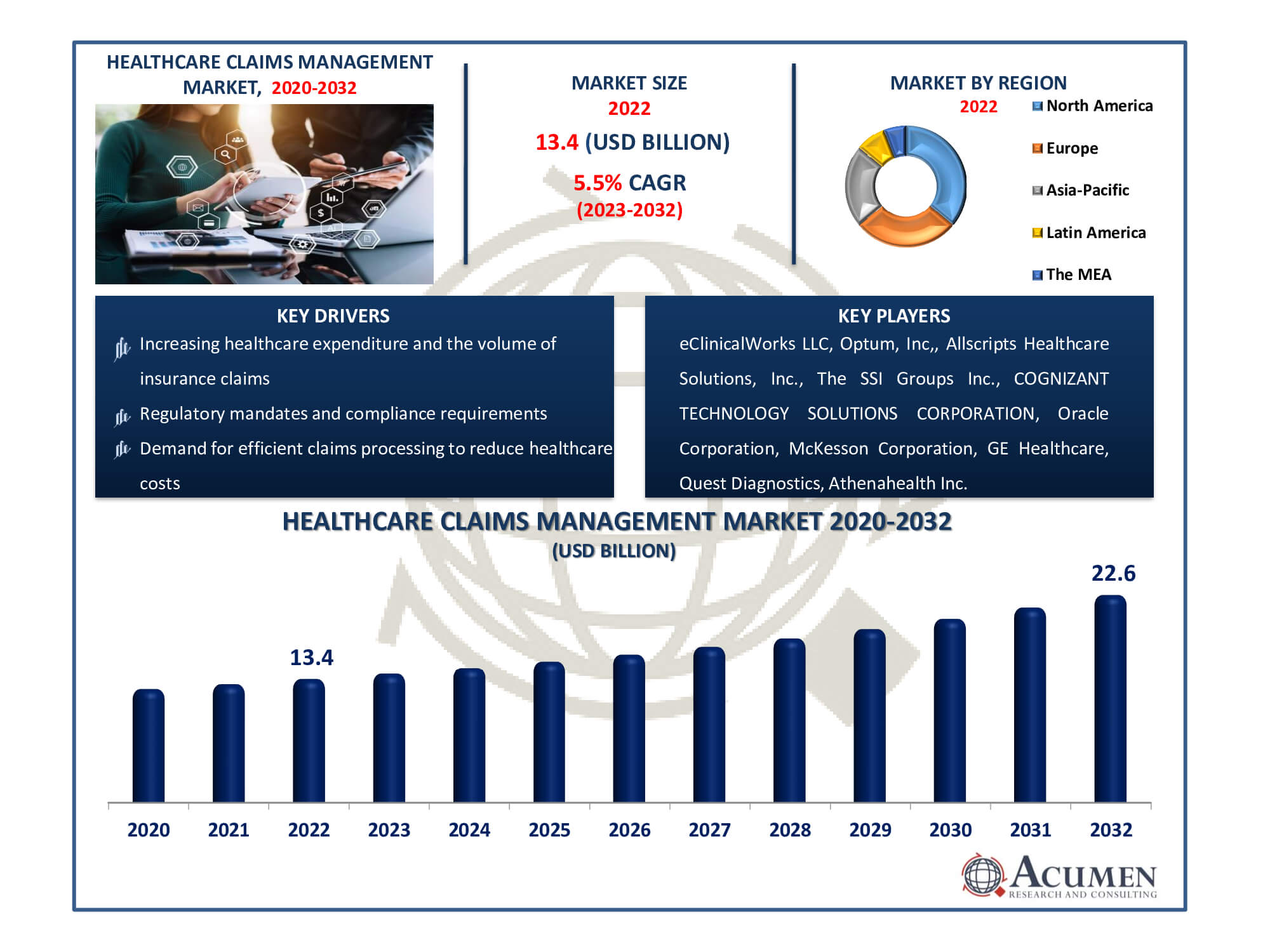
The Healthcare Claims Management Market Size accounted for USD 13.4 Billion in 2022 and is estimated to achieve a market size of USD 22.6 Billion by 2032 growing at a CAGR of 5.5% from 2023 to 2032.
Healthcare Claims Management Market Highlights
- Global healthcare claims management market revenue is poised to garner USD 22.6 billion by 2032 with a CAGR of 5.5% from 2023 to 2032
- North America healthcare claims management market value occupied around USD 4.8 billion in 2022
- Asia-Pacific healthcare claims management market growth will record a CAGR of more than 6% from 2023 to 2032
- Among type, the integrated solutions sub-segment generated over US$ 9.4 billion revenue in 2022
- Based on end-use, the healthcare provider sub-segment generated around 66% share in 2022
- Entry into emerging markets with evolving healthcare systems is a popular healthcare claims management market trend that fuels the industry demand
The market for healthcare claims management is the sector of the economy that deals with the filing, monitoring, and administration of health insurance claims. It includes a number of software programmes and services designed to simplify the difficult and frequently time-consuming process of filing, reviewing, and paying medical claims. Because it ensures accurate and timely claims processing, lowers fraud, and boosts the financial performance of payers and healthcare providers, this market is essential to the healthcare ecosystem. The needs of the business are constantly changing the healthcare claims management market due to the continuous digital transformation and growing significance of healthcare cost control.
Global Healthcare Claims Management Market Dynamics
Market Drivers
- Increasing healthcare expenditure and the volume of insurance claims
- Growing adoption of electronic health records (EHR) and digital health systems
- Regulatory mandates and compliance requirements
- Demand for efficient claims processing to reduce healthcare costs
Market Restraints
- Complex and evolving healthcare regulations
- Data security and privacy concerns
- Resistance to technology adoption in some healthcare organizations
Market Opportunities
- Advancements in artificial intelligence and machine learning for claims processing
- Expansion of telehealth services and remote patient monitoring
- Demand for cloud-based claims management solutions
Healthcare Claims Management Market Report Coverage
| Market | Healthcare BPO Market |
| Healthcare BPO Market Size 2022 | USD 13.4 Billion |
| Healthcare BPO Market Forecast 2032 | USD 22.6 Billion |
| Healthcare BPO Market CAGR During 2023 - 2032 | 5.5% |
| Healthcare BPO Market Analysis Period | 2020 - 2032 |
| Base Year |
2022 |
| Forecast Data | 2023 - 2032 |
| Segments Covered | By Type, By Component, By Deployment Mode, By End-Use, And By Geography |
| Regional Scope | North America, Europe, Asia Pacific, Latin America, and Middle East & Africa |
| Key Companies Profiled | eClinicalWorks LLC, Optum, Inc., Allscripts Healthcare Solutions, Inc., The SSI Groups Inc., COGNIZANT TECHNOLOGY SOLUTIONS CORPORATION, Oracle Corporation, McKesson Corporation, GE Healthcare, Quest Diagnostics, and Athenahealth Inc. |
| Report Coverage |
Market Trends, Drivers, Restraints, Competitive Analysis, Player Profiling, Covid-19 Analysis, Regulation Analysis |
Healthcare Claims Management Market Insights
The rapid increase in the number of patients suffering from chronic diseases and the rise in healthcare claims has driven the demand for healthcare claims management solutions. According to the National Association of Insurance Commissioners (NAIC), in 2018, the direct written premiums of the accident and health insurance industry reached $1.1 trillion, marking a 57.3% increase from 2009. The ten largest insurers collectively wrote 51.8% of the total US market. As healthcare costs rise each year, consumers are increasingly turning to health insurance. With better insurance policies offered by the government, consumers are choosing this secure option.
According to the Congressional Research Service, an estimated 58 million individuals (18.1% of the U.S. population) were enrolled in Medicare in 2019, further increasing the demand for claim management solutions to streamline claims processing. Major players in the industry are focusing on expanding their businesses through strategic acquisitions, which is expected to enhance their customer base and increase their revenue share. This is projected to drive the growth of the healthcare claims management market.
In addition, the introduction of innovative solutions to expand product portfolios is expected to drive the growth of the healthcare claims management market. However, factors such as the high cost of product development and deployment, as well as concerns related to data security, could impede market growth. The shortage of skilled professionals is also expected to pose a challenge to the market's expansion. Nonetheless, the increasing adoption of cloud technology and the integration of AI in healthcare offer new opportunities for market players. Additionally, the rising number of insurance cases and the focus on exploring untapped markets in developing countries are expected to boost the revenue generation of the healthcare claims management market. According to the Current Population Survey Annual Social and Economic Supplement, a significant percentage of people did not have health insurance at some point during the year
Healthcare Claims Management Market Segmentation
The worldwide market for healthcare claims management is split based on type, component, deployment mode, end-use, and geography.
Healthcare Claims Management Types
- Integrated Solutions
- Standalone Solutions
As per the healthcare claims management industry analysis, integrated solutions lead the industry and market forecasts support this trend. These solutions offer a comprehensive approach to claims processing, seamlessly integrating all stages from submission to reimbursement. They enhance efficiency, reduce errors, and ensure data accuracy, resulting in faster claims adjudication. Integrated solutions also facilitate compliance with stringent regulatory requirements, a crucial aspect in the healthcare industry.
Moreover, market forecast indicate sustained growth in the demand for end-to-end automation and interoperability in healthcare claims administration. This aligns with the broader trend of digital transformation in healthcare. As a result, integrated solutions are well-positioned to maintain their dominance in the market, offering healthcare providers and payers a pathway to enhanced efficiency and compliance.
Healthcare Claims Management Components
- Software
- Services
Software dominates the healthcare claims management industry, and market analysis corroborates this trend. Software is indispensable for automating and streamlining the complex claims processing workflow, making it the largest segment in the market. Healthcare organizations rely on robust software solutions to efficiently manage the intricate administrative and financial tasks associated with claims. These software platforms significantly reduce manual labor and errors through functions such as claims tracking, validation, and adjudication. Real-time data insights and analytics empower better decision-making. Software solutions align with the industry's emphasis on efficiency and digitization, reflecting the growing demand for technologically advanced solutions that enhance claims processing speed and accuracy.
Healthcare Claims Management Deployment Modes
- On-premise
- Cloud-based
- Web-based
The Web-based segment of the healthcare claims management market is the largest because of its flexibility and accessibility. Web-based solutions are very handy for healthcare providers, payers, and administrators since they can be accessed from any device that has an internet connection. They lessen the load of software installations and upgrades and do away with the requirement for complicated on-premise infrastructure. Web-based solutions are the chosen option for many healthcare organizations due to their adaptability and simplicity of access, which contributes to their market domination. As per the healthcare claims management market forecast, the web-based category is also gaining traction, bolstered by a deliberate move towards cloud-based solutions for more efficient claims processing. Web-based solutions are being used more and more by the healthcare industry for claims administration because of their affordability and scalability.
Healthcare Claims Management End-Uses
- Healthcare Payers
- Healthcare Provider
- Other
Healthcare claims management is a vital component of the healthcare sector, serving a wide range of end users such as healthcare payers, providers, and other entities. Healthcare payers, including insurance corporations and government health organizations, use claims management systems to effectively process and handle insurance claims. Healthcare providers, such as hospitals and clinics, utilize these systems to improve billing operations, manage payments, and assure proper financial transactions with payers. Third-party administrators and outsourcing organizations that handle claims may fall into the "other" category. While the dominance of a particular end-use may differ by location and healthcare system, healthcare payers frequently play an important role since they handle and process a large volume of insurance claims. According to healthcare claims management market analysis, healthcare payers and providers gain from having simple, remote access to claims data, which facilitates quick decision-making and increased operational effectiveness. This development is consistent with the larger market trend towards cloud-based solutions, which has made web-based platforms the industry standard for healthcare claims management.
Healthcare Claims Management Market Regional Outlook
North America
- U.S.
- Canada
Europe
- U.K.
- Germany
- France
- Spain
- Rest of Europe
Asia-Pacific
- India
- Japan
- China
- Australia
- South Korea
- Rest of Asia-Pacific
Latin America
- Brazil
- Mexico
- Rest of Latin America
The Middle East & Africa
- South Africa
- GCC Countries
- Rest of the Middle East & Africa (ME&A)
Healthcare Claims Management Market Regional Analysis
The largest regional player in the healthcare claims management market is North America, and this significance is attributed to several important factors. First and foremost, owing to its well-established and well-funded healthcare infrastructure, North America has been an early adopter of cutting-edge healthcare technologies, including claims management systems. Second, the region's intricate and heavily regulated healthcare system necessitates effective claims administration, making the use of cutting-edge technologies imperative. Robust claims management systems are in high demand due to the sheer magnitude of the North American healthcare market, which includes a large number of insurance companies and healthcare facilities. Market forecast further affirm North America's leadership in the healthcare claims management market.
In contrast, the region with the fastest rate of growth for the healthcare claims management industry is Asia-Pacific. Its quick rise can be ascribed to the developing healthcare sector, which is supported by the growing middle class, more people having access to healthcare, and an increase in the number of healthcare providers. Specialized claims management solutions are becoming increasingly necessary as healthcare becomes more complex. In addition, the Asia-Pacific area is a favored centre for business process outsourcing (BPO) services due to its highly skilled labor population and reasonably priced labor markets. The demand for claims management services in the region is being further accelerated by the growing adoption of innovative technology and digital healthcare solutions. Due to its dynamic climate, acceptance of outsourcing, and use of new technologies, Asia-Pacific is now the fastest-growing participant in the worldwide healthcare claims management market.
Healthcare Claims Management Market Players
Some of the top healthcare claims management companies offered in our report includes eClinicalWorks LLC, Optum, Inc,, Allscripts Healthcare Solutions, Inc., The SSI Groups Inc., COGNIZANT TECHNOLOGY SOLUTIONS CORPORATION, Oracle Corporation, McKesson Corporation, GE Healthcare, Quest Diagnostics, Athenahealth Inc.
- In 2021, Majesco, a global provider of cloud insurance platform software, acquired ClaimVantage. This acquisition is expected to enable the company to offer next-generation insurance technology solutions, allowing insurers to accelerate their digital transformation to meet the demands of tomorrow. It is anticipated that this move will expand the company's product offerings and enhance its overall business.
- In 2020, Change Healthcare, a global healthcare technology company, acquired the 'PROMETHEUS Analytics' solution from Altarum. This product acquisition is expected to enhance the company's business and increase its revenue share in the global market.
Frequently Asked Questions
The market size of healthcare claims management was USD 13.4 billion in 2022.
The CAGR of healthcare claims management is 5.5% during the analysis period of 2023 to 2032.
The key players operating in the global market are including eClinicalWorks LLC, Optum, Inc., Allscripts Healthcare Solutions, Inc., The SSI Groups Inc., COGNIZANT TECHNOLOGY SOLUTIONS CORPORATION, Oracle Corporation, McKesson Corporation, GE Healthcare, Quest Diagnostics, and Athenahealth Inc.
North America held the dominating position in healthcare claims management industry during the analysis period of 2023 to 2032.
Asia-Pacific region exhibited fastest growing CAGR for market of healthcare claims management during the analysis period of 2023 to 2032.
The current trends and dynamics in the healthcare claims management industry include increasing healthcare expenditure and the volume of insurance claims, growing adoption of electronic health records (EHR) and digital health systems, regulatory mandates and compliance requirements, and demand for efficient claims processing to reduce healthcare costs.
The integrated solutions type held the maximum share of the healthcare claims management industry.